
There was this warning circulated online that a kindergarten pupil died of the deadly meningococcemia in one of the big hospitals in Davao.
“Unfortunately, we were exposed at the emergency room (ER) at the hospital as we were together with the kid who was diagnosed late of having meningococcemia,” the warning said. “The boy died and the doctors were still having a meeting as to what they would do with us who were exposed of this airborne disease.”
When someone asked if it is true, the person who posted the warning said, “It’s confirmed.” Another joiner cautioned: “Please, don’t make confirmation unless stated by the hospital or the city government. My friend, who is a nurse at the ER, told me the hospital is not lockdown. The patient was just transferred. They were just cleaning and the ER is now open.”
But the person who posted the warning insisted that it was true – and that the disease is airborne and even shared an information from a website. The joiner replied: “I get what you mean. But in nursing perspective, post like this can spread more fear and a lot of people might misinterpret the situation. Unless (the warning comes) from the hospital itself and the city government, (it’s another story); their post is more reliable which can be shared.”
The Davao Center for Health Development of the Department of Health urged those who shared the posts in their social media account to be responsible. “Let us not cause alarm nor panic to the public with unverified information,” it urged
Contrary to what the posts claim, meningococcemia’s mode of transmission is through droplet and not airborne, the health department pointed out.
Dr. Richard T. Mata, in a video posted on his Facebook account, explained that meningococcemia is not as highly contagious like chicken pox or measles. “But if you are hit by it, you will die within 24 hours,” he warned.
“Ganun kagrabe ang sakit na iyan,” Dr. Mata said.
“When someone has the disease, the bacteria enter the bloodstream and multiply, damaging the walls of the blood vessels. This causes bleeding into the skin and organs,” the US Centers for Disease Control and Prevention said.
“Meningococcemia is a disease caused by the dissemination of meningococci bacteria, Neisseria meningitidis, into the bloodstream,” explains the website, emedicinehealth.com. “Meningococcal septicemia is another term for meningococcemia.”
The World Health Organization calls it “a bacterial form of meningitis, a serious infection of the thin lining that surrounds the brain and spinal cord.”
Actually, there are three types of meningococcemia: meningitis caused by Neisseria meningitidis, meningitis with Neisseria meningitidis bacteremia, and meningococcemia (Neisseria meningitidis in the blood).
Meningococcemia is contagious and it can be transmitted from person to person. The Department of Health (DOH) said it can spread via direct contact with discharges from the nose and throat that contain the bacteria.
“The bacteria are transmitted from person-to-person through droplets of respiratory or throat secretions from carriers,” WHO said. “Smoking, close and prolonged contact – such as kissing, sneezing or coughing on someone, or living in close quarters with a carrier – facilitates the spread of the disease.”
According to the United Nations health agency, the bacteria can be carried in the throat and sometimes overwhelms the body’s defenses allowing the bacteria to spread through the bloodstream to the brain. “It is believed that 1% to 10% of the population carries Neisseria meningitidis in their throat at any given time,” it says. “However, the carriage rate may be higher (10% to 25%) in epidemic situations.”
A news report from the website of ABS-CBN said meningococcemia is very much endemic in Asian countries, including the Philippines. “Its contamination is seasonal occurring most of the time in colder months,” it said. “A person testing positive to this disease must be incubated for 2 to 10 days.”
The figure cited by the news report is the range, but the average incubation period is four days, according to WHO.
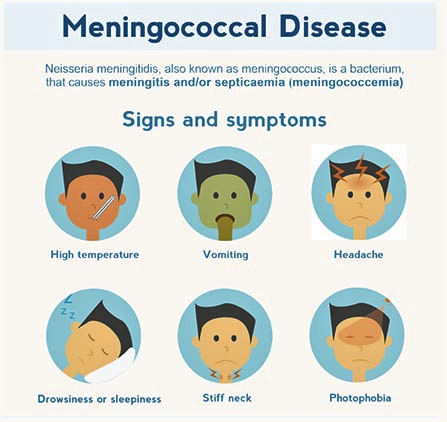
“The most common symptoms are a stiff neck, high fever, sensitivity to light, confusion, headaches and vomiting,” the WHO says. “In addition in infants, bulging fontanelle and ragdoll appearance are commonly found.
“A less common but even more severe (often fatal) form of meningococcal disease is meningococcal septicemia, which is characterized by a hemorrhagic rash and rapid circulatory collapse.”
Meningococcemia may not be highly contagious but it is deadly. “Even when the disease is diagnosed early and adequate treatment is started, 8% to 15% of patients die, often within 24 to 48 hours after the onset of symptoms,” the WHO states. “If untreated, meningococcal meningitis is fatal in 50% of cases and may result in brain damage, hearing loss or disability in 10% to 20% of survivors.”
Most of those who are most likely to be infected with it are children. “Mahina kasi ang resistinsiya ng mga bata,” Dr. Mata said. But adults are not spared. “It is most common in young children,” wrote Jose Antonio Plaza and Victor Prieto, authors of Modern Surgical Pathology. “It occurs rarely in adults.”
As meningococcemia is fatal, it should always be viewed as a medical emergency. A range of antibiotics can treat the infection, including penicillin, ampicillin and ceftriaxone.
“Admission to the hospital or health center is necessary,” the WHO advises. “Isolation of the patient is not necessary. Appropriate antibiotic treatment must be started as soon as possible, ideally after the lumbar puncture has been carried out if such a puncture can be performed immediately.
“If treatment is started prior to the lumbar puncture it may be difficult to grow the bacteria from the spinal fluid and confirm the diagnosis. However, confirmation of the diagnosis should not delay treatment.”
By the way, there are vaccines available to prevent infection by Neisseria meningitidis. – ###






