“We know very clearly by a number of studies that if you treat a person who is infected with HIV and bring down the level of virus to below detectable that not only do you save the life of that person but you make it essentially impossible for that person to transmit the virus to another individual.” – Dr. Anthony Fauci, director of the United States National Institutes of Allergy and Infectious Diseases

As he was skinny and just average in the class, Kevin (not his real name) was not so popular among his classmates in high school. But this changed when he went to college in one of the universities in Davao City.
During weekends, he went to a gym. After a year, Kevin didn’t have only a body to die for but he had become so handsome that he could be mistaken for an actor. He became an overnight sensation. Kevin was seen going out with different girls every week.
To sustain his admiration from girls and for expenses he incurred during those dates, Kevin also went out with closeted homosexuals for one-night stands. He used condom during those trysts but there were instances when he was so drunk that he could not wear the protection.
Upon graduation from college, Kevin was set to conquer the world literally. He applied for a job abroad and one of the requirements was to undergo a medical examination, including HIV (human immunodeficiency virus) test.
He did. After going through with the process, he was given the result. When he received it, he felt as if the world seemed to collapse. He was positive for the virus that causes Acquire Immune Deficiency Syndrome (AIDS).
Kevin’s case is not part of the statistics of HIV/AIDS and ART (anti-retroviral treatment) Registry of the Philippines. In June of this year, 1,006 people have been confirmed to be carrying the dreaded virus. Nineteen percent (194) had clinical manifestations of advanced HIV infection.
From January to June, the epidemiology bureau of the Department of Health recorded 6,372 cases – bringing a total of 68,401 cases since 1984, the time the country reported its first case.
Most of those infected were through sexual contact, particularly male to male sex. The June data showed 589 men (59%) were infected through this kind of sex while another 260 men (26%) got the virus through sex with both males and females. Only 134 people (13%) were infected through male to female sex.
HIV infection is growing through the years, records from the health department showed. From one case in 2008, it went up to 7 cases per day in 2011, 16 cases per day in 2014, and 32 cases per day in 2018. From January to June this year, there are 35 new cases each day.
In Davao City, the Reproductive Health and Wellness Center (RHWC) reported a total of 39 new HIV cases from January to February this year. That’s about 19 cases per month and most of them obtained through sexual intercourse.
Kevin must have not heard of transactional sex. These are people who engage in this kind of sex either pay for the service or accept payment for sex or both. In June 2019, 12% (123 cases) of the newly diagnosed engaged in transactional sex.
It’s a long way to go for those people living with HIV/AIDS. “Workers and employees in the Philippines living with HIV who suffer workplace discrimination often do not seek redress,” Human Rights Watch (HRW) said in a statement. It added that the government’s response to unlawful firings and harassment is “weak.”
Take the case of a 26-year-old Elizabeth (not her real name), another HIV-positive. A single mother of a 6-year-old boy, she worked as a cashier at a café. When she learned about her status, she was totally devastated. “I cried all the time, every time I’m reminded of what happened,” she said, adding that she cried even more “because of the discrimination I’m going through.”
Two years after she was diagnosed of having HIV, Elizabeth started to suffer from double vision and frequent headaches. Her doctor, who could not determine whether she was suffering from an opportunistic infection, suggested that she undergo an MRI on her eyes.
Because the doctor recommended rest, she needed to file a leave of absence from her company. “I told our human resources about my status so I can have a valid excuse for my leave, which was going to take a long time because the doctor wanted me to rest,” she said.
She was fired as a result. “My supervisor said she understood me and would like to help,” she said. The supervisor then referred Elizabeth to the manager of a manpower company that supplies workers for restaurants. The manager told her: “Since there may be people who won’t understand what happened to you, I need to pull you out of the coffee shop.”
The manager then asked Elizabeth to fill out forms, one of which turned out to be a resignation letter from employment agency, not just the coffee shop. “I asked why and he told me it’s because I was exposed to food,” she said. “He was very good at convincing me to resign for my own good, that resigning would reduce my stress, things like that. But it was painful. I know what he was asking me to do was wrong. It felt wrong.”
At the manager’s urging, she signed the resignation letter.
Stories like this abound. So much so that in Davao City, the government is trying to help those PLWHA. In fact, Mayor Sara Z. Duterte has signed the Davao City Comprehensive STI, HIV and AIDS Ordinance of 2013. STI stands for sexually transmitted infection.
With a commitment “to fight against the epidemic,” Ordinance No. 0679-19 aims to “prevent the spread of HIV and other STIs and mitigate any related social, psychological, and economic consequences.”
Through the ordinance, the Davao City AIDS Council (DCAC) has been formed with the mayor as the chairperson and the City Health Office as co-chair. Members include SP Committee on Health, City Social Services and Development Office, Department of Education Davao City Division, Chair of the Liga ng mga Barangay, Integrated Gender and Development Division, City Information Office, City Department of the Interior and Local Government, and Sangguniang Kabataan.
Five more members come from the non-government organizations, namely: LGBT, faith-based organization, PLHIV, entertainment industry and indigenous people’s representative. Another five members come from line-national agencies working on STI, HIV/AIDS prevention.
The ordinance has come up with several initiatives. For one, it will conduct STI, HIV/AIDS awareness campaigns, especially during the months of January, May and December (as World AIDS Day is commemorated on the first day of this month).
Another program is conducting age-appropriate HIV and AIDS education in schools. Section 9 of Article IV states: “to integrate basic and age-appropriate instruction on causes, modes of transmission on STI, HIV and AIDS, national and local HIV related laws and other related issues of stigma reduction and discrimination in the workplace, public and private, including the Armed Forces of the Philippines and the Philippine National Police.”
The ordinance likewise conducts HIV and AIDS education in communities, among out-of-school youths and those going abroad. On the latter, Section 12 of Article IV explains: “all overseas Filipino workers shall be provided with information on how to access on-site STI, HIV and AIDS-related services and facilitates before certification of overseas assignment.”
OFWs are not spared from HIV infection. “Sixty-one Filipinos who worked overseas within the past five years, whether on land or at sea, were diagnosed in June 2019,” the health department reported. “They comprised 6% of the total newly diagnosed cases for the month.”
HIV/AIDS is one of the most dreaded diseases ever known to human beings. “A single sexual encounter can be sufficient to transmit HIV,” wrote Dr. John Hubley, author of The AIDS Handbook. “Although the risk from an individual sexual act may be low, the more times a person has sex, the greater the likelihood that transmission will take place.”
Injection or infusion of contaminated blood, as occurs with blood transfusions, the sharing of needles or syringes, or an accidental prick from an HIV-contaminated needle is another mode of HIV transmission.
Transfer of HIV is also possible from an infected mother to a child before birth, during birth, or after birth through the mother’s milk. “A few children contract HIV infection through sexual abuse,” informs The Merck Manual of Medical Information.
In theory, medical experts say it is also possible, although extremely rare, for HIV to spread through oral sex (only if there are bleeding gums or open sores in the person’s mouth), being bitten by a person with HIV (only if saliva is bloody or there are open sores in the person’s mouth), and contract between broken skin, wounds, or mucous membranes and the blood of someone living with HIV.
The website, healthonline.com, points out that HIV is not spread through: skin-to-skin contact; hugging, shaking hands, or kissing; sharing food or drinks; saliva, tears, or sweat (unless mixed with the blood of a person with HIV), sharing a toilet, towels, or bedding; mosquitoes or other insects; and air or water.
“HIV is a virus that destroys the immune system,” says Dr. Louie Mar A. Gangcuangco, an infectious disease researcher whose expertise in HIV field is recognized internationally. “This is something we should be concerned about. After about 5 years of not knowing that you are infected, if you engage in unprotected sex, the infected person can unwittingly transmit the virus, infecting more people.”
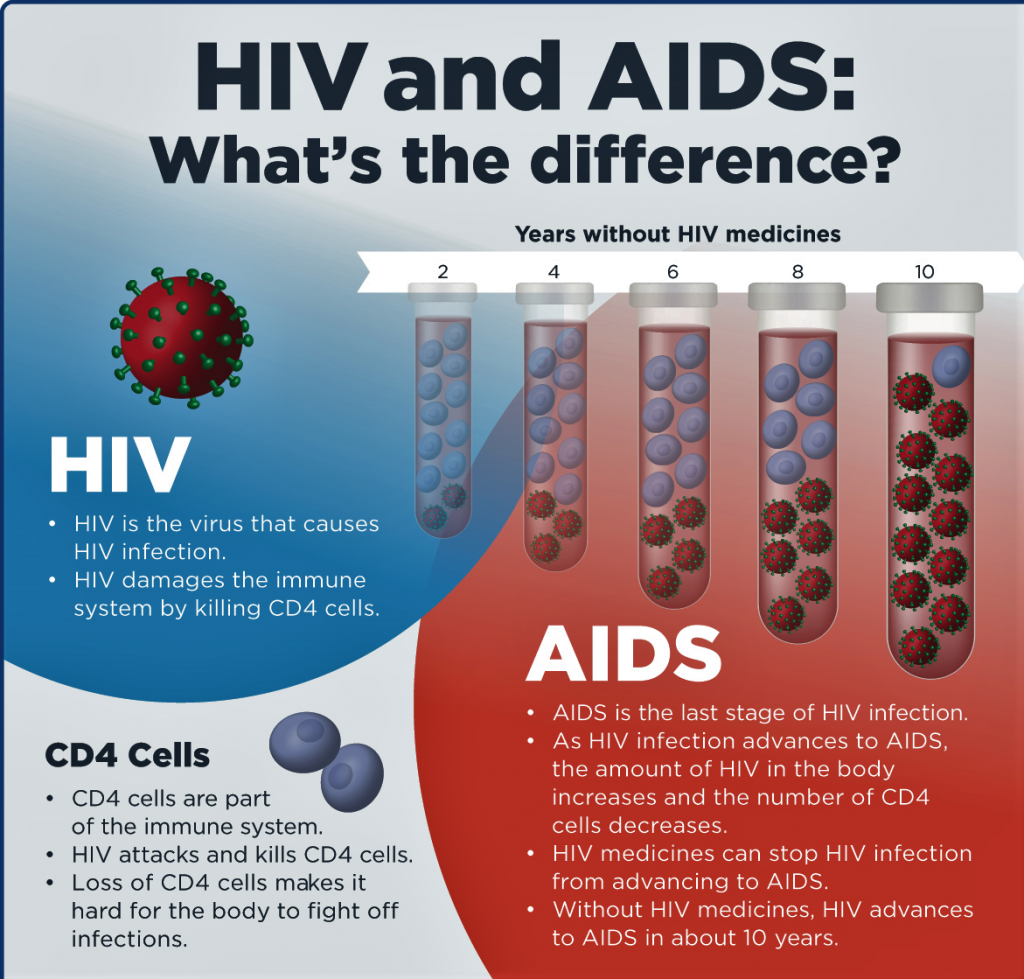
AIDS is the most advanced stage of HIV infection. “This can take from 2 to 5 years to develop, depending on the individual,” says the World Health Organization (WHO). It defines AIDS as “the development of certain cancers, infections, or other severe clinical manifestations.”
A person with HIV will never know he is positive of the virus unless he or she undergoes an HIV test. “Having an HIV test is the only way to know for sure whether you have HIV,” said the website,www.aidsmap.com. “If you have HIV, it’s very important that it’s diagnosed. This will give you the best chance of getting the treatment and care you need to stay well.”
The Davao City HIV/AIDS ordinance said DCAC shall ensure confidentiality in all matters pertaining to the disease as provided for in the National AIDS Law and other related policy issuances.
It added that those who are tested positive to HIV “is obliged to disclose his or her status and health condition to his or her spouse or sexual partner prior to engaging in penetrative sex or any potential exposure to HIV.” The HIV-positive person may also “opt to ask help from health providers in case of disclosure.”
Currently, there is no cure known for HIV but the virus can be controlled with proper medications called antiretrovirals. “These antiretrovirals are provided for free by the government,” Dr. Gangcuangco says. “With healthy lifestyle and if antiretrovirals are taken every day, people with HIV can have ‘undetectable’ virus in their blood.”
By “undetectable,” he means that the virus is still in the body but in very low amounts that it cannot be detected by the machine.
According to Dr. Gangcuangco, there are two benefits of taking medications for HIV. First, it prevents HIV from destroying the immune system of someone with the virus. Second, it prevents the spread of HIV because the virus will also be very, very low in the semen and other body fluids.
Another good news: there is now a medication, when taken every day, can prevent HIV infection. It is called pre-exposure prophylaxis (PrEP for short). “This medication is a pill that contains antivirals,” explains Dr. Gangcuangco. “When HIV enters the body, a person who takes PrEP is protected against HIV infection. PrEP blocks the virus from reproducing in the body and is effective to prevent HIV transmission by more than 90%.”
Some years ago, the United Nations health agency issued a statement that said: “People at substantial risk of HIV infection should be offered PrEP as an additional prevention choice, as part of comprehensive prevention.”
Dr. Gangcuangco, however, dispel the idea that PrEP can now replace condoms and other preventive measures for HIV. On the contrary, PrEP should be offered together with them. “PrEP is not meant to replace counseling and condom use but should be used as an adjunct to prevent HIV,” he explains.
According to the boyish-looking physician, HIV is not and should not be treated as a death sentence anymore. “If HIV is detected early and if the patient takes antiretrovirals early,” he says, “the virus can be controlled. There is still no cure for HIV but the bad effects of the virus can be prevented if medications are taken early.”
His final words: “I urge everyone who has had unprotected sex to please have an HIV test in your nearest HIV treatment hub/social hygiene clinic. People with HIV need to get tested to prevent damage to their immune system that can cause infections such as pneumonia, tuberculosis, diarrhea that can lead to death. – ###
(Photos taken from the net)






